This is the third post in a series on my experience as a stem cell donor. If you missed them, check out Part 1 and Part 2.
As I’ve talked with others about the stem cell donation process, I’ve realized most of us are woefully uneducated! There are far too many people waiting for a donor because there's no known match--especially in non-white ethnicities.
The goal of the series is simple: increase awareness, reduce fear and misconceptions about being a donor, and help save lives.
I’ve set out to share my experience as a stem cell donor—the good, the bad, and the ugly! This isn’t the most entertaining topic, but it’s an important one.
Buckle up–this could get bumpy. There are some photos that may show bandages and blood–not open wounds or anything, but if you don’t like looking at blood of any type, perhaps just skip to the recap or skip reading the post and listen to the voiceover instead.
Here we go!
As we left home to head to Little Rock for the stem cell donation last month, I saw that my brother (who is more of a consumer of social media than a sharer) had posted an update.
“UPDATE:
I got all of my appointments done Monday to get clearance for my transplant as well as admittance into my room late Monday evening. I started my chemo yesterday and will have another chemo added after midnight tonight. In a few days I will have a third concoction added that comes from animals (rabbits). I’ve learned…don’t ask no questions, just go with it.
I am scheduled to receive my transplant next Wednesday and that will be considered my ‘Day 0.’ I will have no immune system for several weeks afterwards, so prayers that the infections stay away. Thank you for all the prayers, thoughts, and messages. Prayers for my sister and her husband Mike, as they will be arriving tomorrow eve to start her stem cell collection process Friday. #1, I want them to have a safe trip. #2, I need my stem cells to get here…”
See his real reason for praying for my safety?? He only loves me for my stem cells.
I quickly commented with jokes of my own.
And you know I couldn’t let the rabbit thing go without a couple of digs (we continue to have big laughs over the rabbit thing). It’s true–he was given antibodies derived from rabbits to prevent graft-versus-host disease. Sounds weird to me, but hey—all of this has been mind-blowing. What’s a few rabbits thrown in the mix?
When we arrived, we checked into our Airbnb and unloaded the vehicle before going to the hospital to visit Van. Gowns and gloves were required in addition to our masks due to risk of infection. He was on his third day of chemo but was feeling okay and was upbeat. It was great to spend a little time joking around with him–a perk of knowing the transplant recipient. Seeing him definitely furthered my resolve to power through any discomfort during the process.
Friday - Day 1
We arrived at the Winthrop P. Rockefeller Cancer Institute around 8 a.m. I forgot the appointment schedule the coordinator sent me (yeah, I know–kind of important), but the staff at the front desk quickly printed it and pointed me in the right direction. We took the elevator to the sixth floor to Infusion Center B.
After checking in, we waited a few minutes until a patient care tech called my name. Taria took my weight (ugh) then led us to a small room where she took my blood pressure standing and sitting. Then she said, “Pull down your pants,” as she grabbed the thermometer.
<blink> <blink> “Excuse me?”
“Pull down your mask.”
“Oh…” Mike and I conferred later on this and he was also quite sure she said “pants” not “mask.” All I know is that rectal temperature was not included in any of the literature I received and could very well have been a deal breaker for this donation.
Anyway, we soon met Judy, one of the nurse practitioners for transplants. She drew blood and sent the sample on its way. We had to wait for the results of the test before I could receive my first injection because they have to be 100% certain there is no pregnancy. I quickly told her that if the test came back positive to just send me over to the psych ward of the hospital1.
While we waited, Judy gave me business cards with phone numbers for herself and the other two nurse practitioners in case I had any questions during the process. She also gave me a paper explaining the medication I would be given, potential side effects2, and an after-hours number to call with questions. I felt confident that I had all the information I needed.
The results were finally in–not preggers!--so they called for the pharmacy to send up my first injection of ZARXIO, which is a brand name for filgrastim (another common brand is Granix). “Filgrastim is used to stimulate the production of granulocytes (a type of white blood cell).” Why? The bone marrow goes into overdrive then becomes too full of cells, so the excess cells spill over into the bloodstream where they can be collected in a much less invasive manner than having to collect directly from bone marrow3.
The injection arrived. I had been apprehensive about this moment since I learned it would be given in my stomach. Typically I’m am fine with shots in the arm or derrière or with blood draws–I usually watch the needle going in. However, the thought of a shot in the stomach didn’t sit well with me.
I was sweating a bit as Judy administered the injection, but my nervousness disappeared within a few seconds—it wasn’t bad at all! In fact, I bragged about how it didn’t really hurt and joked that all that extra padding I had must have helped.
I returned at 4:30 p.m. for a second injection–no issues with that one either, although they downgraded me from a private room to something akin to an office cubicle with half walls. In fact, most of the infusion center was open and filled with the “cubicle stations” along the perimeter with the interior consisting of nurse stations and some rooms.
Around 5:30 p.m. while visiting Van, my hips and legs began to hurt, which was listed as a possible side effect of the ZARXIO. After we returned to our Airbnb, I ate, took Tylenol, and soaked in a hot bath–no issues sleeping.
Saturday - Day 2
My luck ran out. A male nurse administered the 8:30 a.m. injection, and his technique seemed to be very different from that of the nurses on Day 1. My text to my brother said, “That <not-nice word> threw that thing at my stomach like he was playing darts.” It stung and continued to hurt for about an hour after. There was even a bit of a bruise there later.
When I went for my 4:30 p.m. injection, the nurse said, "Your white blood cell count is WAY up!"
I said, "That's what we want, right?"
She said yes, but they normally don't see someone's jump as high this fast. My count jumped from 6k before beginning injections to 40k after only two injections. Exciting news that gave me a morale boost! The afternoon injection was okay, but I began getting achy again around 6pm. I took more Tylenol and had another nice soak in the tub.
Sunday - Day 3
Day 3 had minimal bone pain/aches, but my energy was very low. Between the morning and afternoon injections (both went well–no darts!), Mike and I drove to a local state park. Simply getting out of the vehicle and walking about ¼ mile to an overlook left me wiped out!
Monday - Day 4
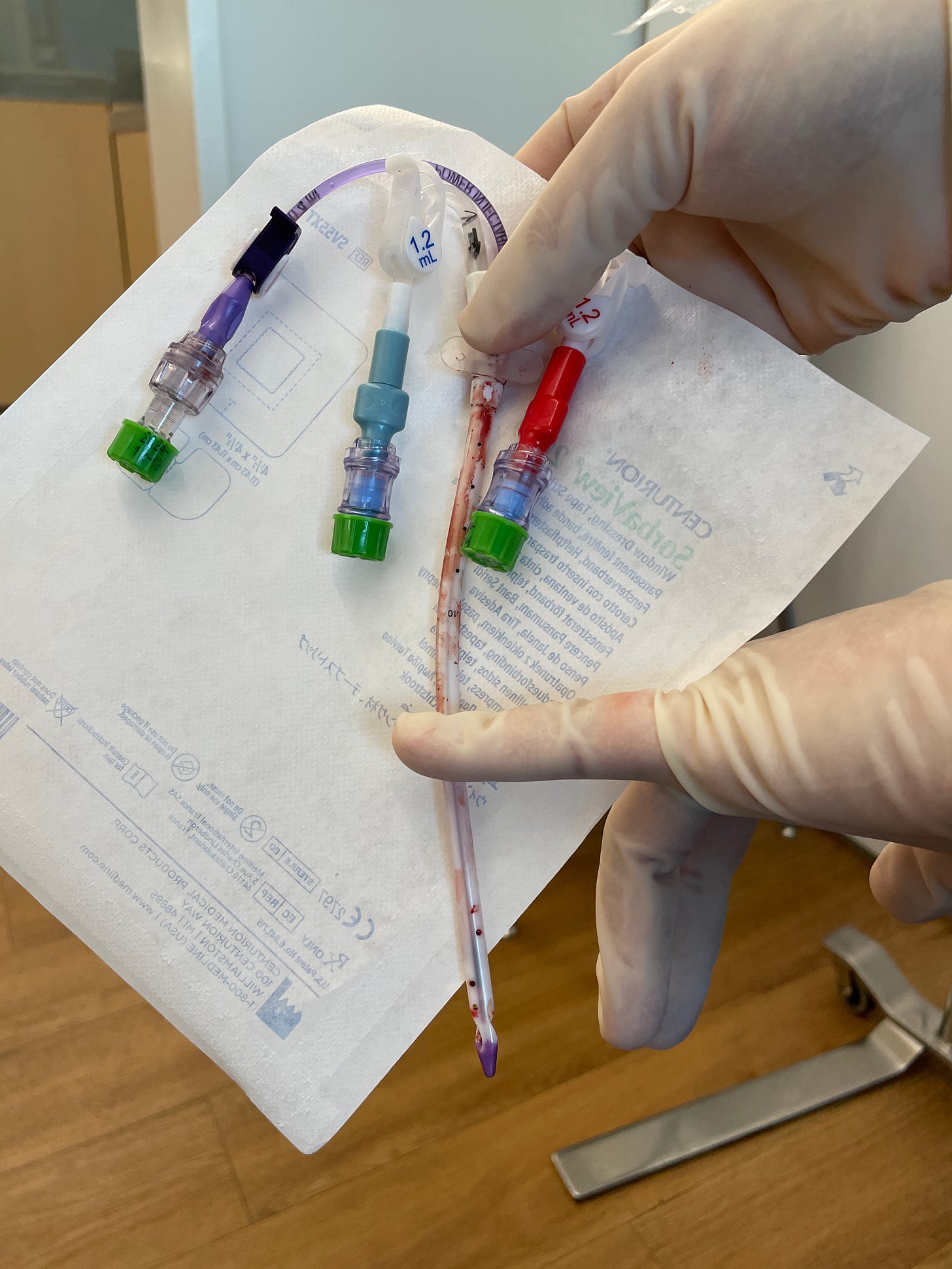
Injections went fine on Day 4, but I also had the line placed in the morning. “The line” as it was commonly called is a Quinton catheter or a vascath. If you’re interested in the details, you can read all about it here. but here’s an image to help you picture it.
I knew practically nothing going into the procedure except where it would be inserted. To be fair, the staff gave me the option to look at the line before they put me on the table and prepped me. I declined. I’m still glad I didn’t look.
My face was covered by a lightweight drape. The doctor introduced himself when he came in and told me to expect a stick, some burning from the lidocaine (to numb), and some pressure as he inserted the line.
I felt the stick—not pleasant, but not awful either. Then came the burning. The doctor was talking as though I wasn’t there, obviously teaching someone as he began inserting the line. For this nervous patient who just wanted it done ASAP, every second counted, and I was getting really peeved. I get that it’s a teaching hospital, but can’t they do that chit-chatting with patients who are under sedation?!4
I felt the pressure as he pushed the line in. Very shortly after, I felt fluttering in my chest, like a hummingbird had gotten in and was bouncing around in there. Queue anxiety attack (as a child/teen I regularly experienced anxiety attacks, some of which were induced by feeling flutters in my chest, which I later learned were heart palpitations).
I’m sure the doctor sensed my discomfort. He asked if I was okay, and I said something (don’t remember what). He said several times, “You shouldn’t feel any pain—just pressure.”
“I know that, and it’s not pain. But I feel fluttering in my chest. It just feels <obscenity> weird!” I may not have said this in my kindest voice.
At that point he stopped talking so much and got down to business. He quietly said something to his apprentice and changed course on the line. The fluttering went away.
After it was done, the doctor came over to where he could see my face under the drape and asked if I was okay. He said something about my vein being very sensitive so he backed the line out and went to a larger vein.
All’s well that ends well, but I had fingernail indentations in the palms of my hands half an hour later when Mike and I sat down at the hospital café to get a bite to eat.

The line was not comfortable, and the area around it was extremely sore. I had trouble getting comfortable that night, and Mike had to hold my head/torso and lower me onto the pillow because engaging my neck muscles hurt like hell when I tried to do it myself.
Tuesday - Day 5
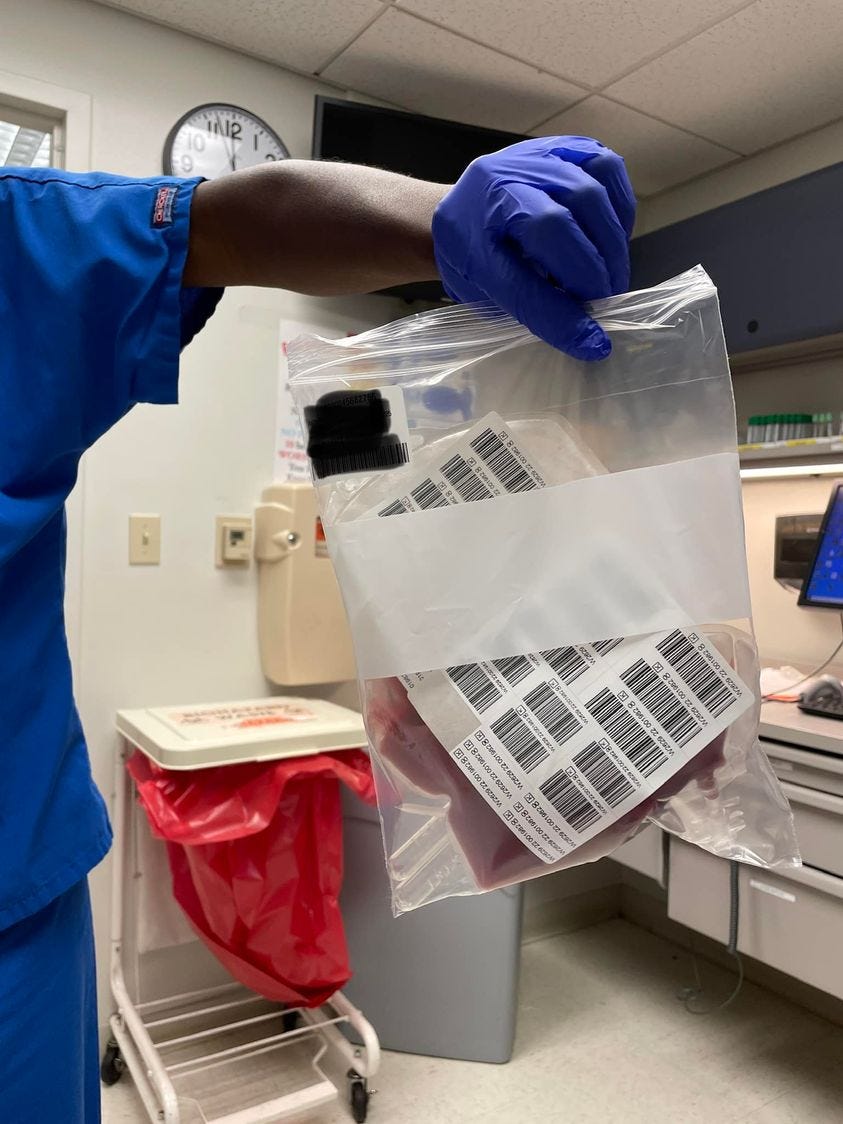
Collection Day finally arrived! I finally understood the reason for the Quinton line—it allows blood to flow both from your vein and back into your vein at the same time. That’s kind of important, right? Collection was a breeze. The machine was a bit loud, but it had a rhythmic clack to it like a train.
Collection took about four hours then we went to visit my brother again and wait for the call—did they get enough, or would I have to go back for another round the next day? A couple of hours later the phone rang:
“We hoped to collect 5 million cells, and we got 5.6—so you’re good to go! You can head over to the infusion center to have your line removed.”
We all rejoiced in Van’s room then Mike and I booked it over to the Cancer Institute. With any luck, we’d be home before 9 p.m.
<sigh>
Nope. It took two hours to get the line removed. About half of that was spent waiting for a nurse to become available and to get everything ready. Was I nervous? A little. But the removal was being performed in one of those open-air cubicle things I mentioned earlier, so how bad could it be, right?
Before the removal, she told me to take two deep breaths then take a third and hold it. I closed my eyes and took three breaths and held it. I felt her tugging and at some point began wondering how much longer before I can come up for air?
Finally, I opened my eyes, and the look of horror on Mike’s face made me wonder if my entire vein had come out with the thing! Later he explained that he was just shocked by the size of the line itself. He had no idea how large it was in length or diameter.
The nurse had to hold pressure for about 15 minutes after the line was out, which hurt because that area was already sore. I then received all these instructions:
what we should do if it began bleeding (apply pressure then go to an ER)
changing the dressing after 24 hours
don’t let the scab come off until it was ready
I felt a little unqualified for all this aftercare, but we were on our way by 5 p.m., ready or not.
Days Following
The days following had a few minor discomforts. I remained tired for several days, and the adhesive from the bandage really did a number on my skin. Overall (and compared to that line install!), it wasn’t bad.
Let’s recap the discomforts.
Recap
Day 1 - general nervousness over the injections; aches in hips and legs in the afternoon
Day 2 - first injection of the day stung (maybe due to technique or hitting a nerve?) and hurt for about an hour; aches in hips and legs in the afternoon.
Day 3 - very low energy just walking any distance
Day 4 - the Quinton line installation. Not good!
Day 5 - the Quinton line removal. Also not fun!
Days Following - some soreness; skin irritation from the bandage adhesive; tired for several days.
Would I do it again? Totally. My brother is now three+ weeks post transplant and is doing very well.
Would I do it for a stranger? I would, but they would have to knock me out for that Quinton line!
I hope this has helped someone in their exploration of becoming a potential donor. The discomforts were small when you consider the potential to save a life. Please consider signing up to be a possible donor at Be The Match.
Seriously. I’m 47, and my youngest child is almost 21 and has given me a run for my money. No more babies, please!
The most common side effects are headaches and bone pain, but you can read all of the possible side effects at the ZARXIO website.
The American Cancer Society has a great article on the different types of donation.
I love using “?!” and recently learned it’s called an interrobang, a word that makes me happy.










1- Holy shit, that was a ride. And good on you for helping your brother when he needed it the most.
2- New life goal: work "interrobang" into every conversation I possibly can.
It seems like it was successful. Well done, best wishes for your brother!